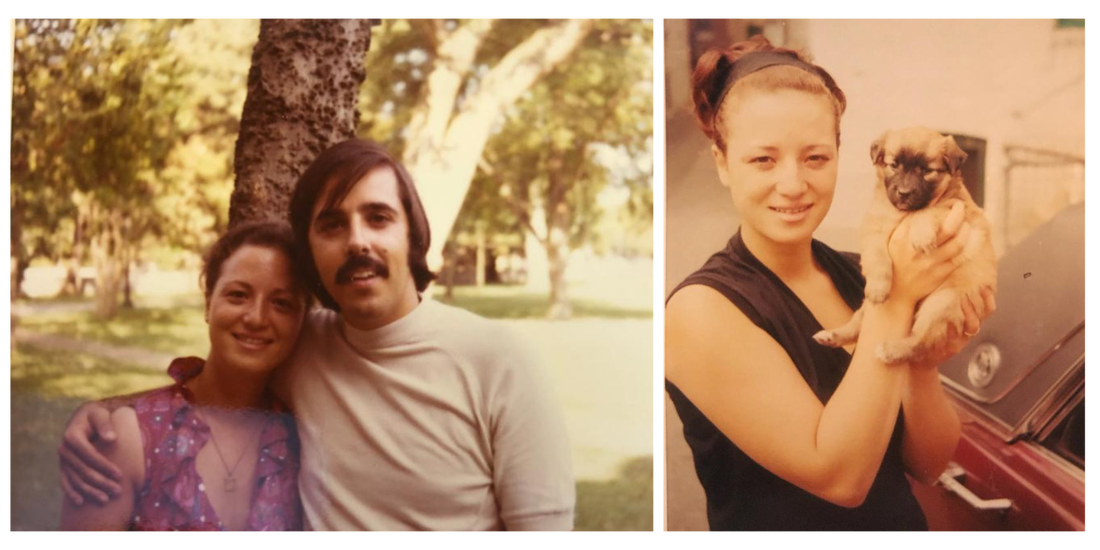
Introduction from Encephalitis411Encephalitis is a serious and sometimes fatal medical emergency. Most do survive the acute stage, particularly if the diagnosis is made promptly and appropriate treatment is initiated before the inflammation causes irreparable brain damage. But as many in our community know, making it past the acute stage of the illness only marks the beginning of the long journey to recovery. Further still, there are some patients who never truly recover. The inflammation may have been so severe that long-term health complications arise, a situation which few are equipped to handle. The result is often a confusing and agonizing journey for caregivers to search for answers, and find follow-up medical care, in an attempt to “get their loved one back.” We at Encephalitis411 know all too well of the additional layers of devastation and heartbreak this causes. For those who have battled through the ugly realities of the encephalitis journey, you’ll find a poignant sense of familiarity in Catie Duggan’s words below. She bravely shares her story not only to honor the memory of her mother, Rae, who passed away a year ago today; but to raise awareness and advocate for improved standards of medical care. Please join us in carrying forward Rae’s positive and courageous spirit, and using Catie’s strength as a catalyst for positive change in the fight against encephalitis. If you would like to write a story for our blog, join our fundraising committee, volunteer, or have your loved one honored on our In Memoriam page, please email us at [email protected] . Catie, please know that you are making a powerful difference through your advocacy and that our community stands together with you with heartfelt condolences and love. 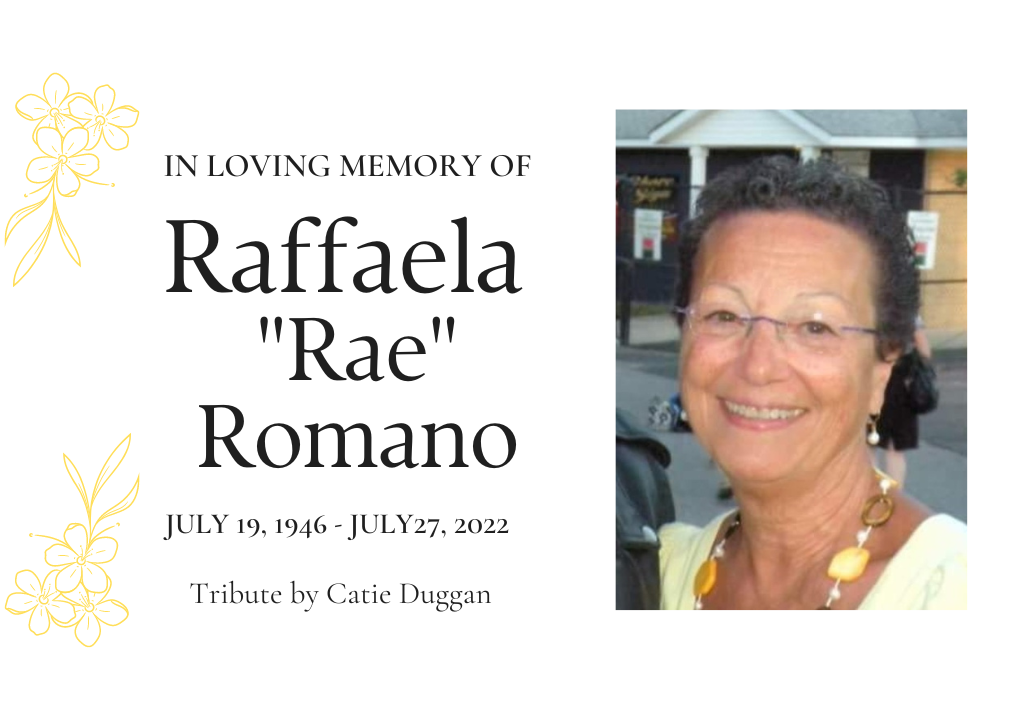 This is my story about my mom’s journey with encephalitis, and her slow decline following her diagnosis and the professional inadequacy of care that we received throughout the 19 months that she courageously battled, until her death on July 27, 2022. On December 23, 2020, I received a text from my dad saying that my mother woke up in the middle of the night, mumbling, confused and disoriented, wandering throughout the house. A few days prior she was complaining of a stiff neck and headache. Concerned, he called an ambulance. My mother was taken to Montgomery General Hospital in Olney, MD where she stayed for the next seven days. Once admitted, an infectious disease doctor was notified of her behavior and began to run tests including a spinal tap. My mom’s brain was inflamed. She was diagnosed with herpes encephalitis. What? I had never heard of herpes encephalitis before. Without hesitation, I looked it up and what I found sent instant shivers throughout my body, my heart began to pound and I wept. I was overcome with fear and worry. I read that, “Herpes simplex virus (HSV) is the most common cause of encephalitis (brain inflammation) in developed countries and is the most treatable of all types of infectious encephalitis. But swift diagnosis and treatment are critical as there is a high mortality rate if left untreated for more than 48 hours. With treatment, the mortality rate is 30%; without treatment, the mortality rate is 70%.” ~Encephalitis 411 Was my mother’s encephalitis treated in time?, I wondered. I wanted to be with her immediately but covid restrictions wouldn’t allow visitors. Sadly, telephone calls were as good as it was gonna get. The conversations I had with my mom were… interesting. I knew that something was different about her the first time we spoke. She would talk in a whisper as if she was hiding a secret from her “friends” who worked at the hospital, yet tell me that they were mean and aggressive, before rushing me off the phone. Another time she claimed she could see my brother Christopher out the window, yet my brother was not at the hospital. I soon learned that delusions and hallucinations can follow the initial onset of encephalitis and that brain damage in adults (and in children beyond the first month of life) is usually seen in the frontal lobes (leading to behavioral and personality changes), and temporal lobes (leading to memory and speech problems). The damage can be severe. A week later, my mother returned home from the hospital. Her brain inflammation was alleviated with the administration of IV acyclovir which was given within the first few days at the hospital. My father became a full time caretaker upon her return and continued to administer the IV acyclovir at home, with the help of a special nurse that would visit occasionally over the next few weeks. We were hopeful and relieved that she was home, but scared not knowing what to expect. She seemed happy for a little while, but we began to notice odd behavior, like putting her pants on backwards or placing items where they did not belong. She was unable to write legibly or remember certain things, like knowing what a toothbrush was, but not understanding how to use one. She suffered with severe anxiety and restlessness that would not let her body or mind rest, often resulting in sleepless nights. Her symptoms were worrisome to her which exacerbated her anxiety. She knew something was wrong. My father and I took her to see her PCP and visited with a neurologist, neither of whom knew hardly anything about encephalitis. The neurologist performed an initial cognitive impairment test, EEG and neuropsychological exam all which were seemingly “normal” for her age, with no concerns. After months of meetings with the neurologist, and bypassing our observations, he insisted that more time was needed and that her anxiety needed to be under control, until further evaluations could be done. It seemed that she was merely being treated as another elderly patient with early signs of dementia. The doctors just weren’t getting it. She began speaking with a neuropsychologist and a psychiatrist who prescribed her a cocktail of psychiatric medication that simply masked the underlying conditions without understanding the complexity of what she was experiencing. My brother Christopher and I would accompany my dad to the doctor’s with her. One of us would speak to the doctor, while the other would walk my mother outside the office, making every effort to distract and calm her mind. I came to learn about the chronic phase of encephalitis, when the brain is no longer inflamed. Doctors can only offer survivors symptomatic management as there is no specific treatment to reverse the brain damage. On top of the anxiety and restlessness, the list of ongoing symptoms was a daily struggle for my mother: physical pain throughout her entire body, depression with bouts of crying, obsessive thoughts, extreme confusion, aphasia, bizarre conversation, paranoia, migraines, I could go on…. We became concerned that the medications were making her behaviors and short-term memory worse, and near impossible to discern the brain damage from the side effects of the medications. I longed for clarity and wanted my mother to detox and be observed to understand first hand what we as a family were noticing. My mother was admitted to Johns Hopkins where I stayed by her side with the help of my sister-in-law, giving my dad a much needed reprieve. I requested that further testing be done to rule out follow-on autoimmune encephalitis. After another spinal tap, CT-scan and a psychiatric evaluation, my mother was released after a 10-day stay with no additional findings. Her body was healthy. They adjusted her medication, but the behavioral improvements didn’t last long and her conditions continued to worsen. Over the next year, my mother was in and out of different hospitals every few weeks. My father did everything he could to care for her and hired a few in-home nurses, but the chronic symptoms my mother experienced were beyond the nurse's training or capabilities. It seemed that there was nothing any of us could do to alleviate her unwanted thoughts and behaviors, or any medicine or cathartic coping skill to comfort her. I realized that there was no answer to understanding the aftermath of an inflamed brain and that my mother’s journey with encephalitis was unique. After 16 months as primary caretaker, I understood my father’s painful decision to move my mother into an assisted living facility. She struggled and courageously fought a long battle until the Lord called her home just 3 short months later. If you had the pleasure of knowing my mom, you knew from the moment she greeted you with her sweet smile and thick New York accent that you were welcomed. She was a fun loving, positive woman, making friends everywhere she went and always had a funny story to tell. Her affection with hugs and kisses, no matter who you were, and generous love for her family was unmatched. She was a woman of faith and kept her faith in God till the very end. My mother, Rae, was a beautiful soul whose brain did not recover from the chronic phase of encephalitis, and who left this Earth too soon. What’s truly scary is that encephalitis does not discriminate by age, sex, or prior health status; it is a serious and sometimes fatal medical emergency that strikes without warning. 20,000 people are diagnosed with encephalitis in the U.S. each year, yet 8 in 10 people don’t even know it exists. Heart strickenly, my family and I learned first hand that lack of awareness extends even to medical professionals: patients are often misdiagnosed, resulting in delayed treatment, decreased recovery potential, and worse quality of life outcomes. This needs to change. Please help spread the word about encephalitis in honor of my mother Rae, and help to improve the wellbeing of all lives touched by this devastating illness. This applies not just to encephalitis survivors but also to anyone who comes in contact with them, including their family and friends. Donations support research, awareness, and advocacy initiatives that improve the quality of life for those impacted by encephalitis. Thanks to your generous contributions over the past decade, Encephalitis411 has directly helped thousands of encephalitis patients, caregivers, doctors, and other community members across the globe!
We appreciate your support.
0 Comments
Introduction
I enjoy reciting my poems to others and have finally accepted that I have to read them from the printed page, however much I would love to recite them from memory. Funny thing this post-encephalitis life (over twenty years now) —the brain working well enough to write the words but not well enough to remember what’s been written! You’ll be pleased to know I now spend less and less time screaming at the moon and very little wallowing in the once was me. Rob, thank you for sharing this powerful piece with us! You've not only boldly articulated your personal experience, but given a voice to countless others afflicted by the same post-encephalitis challenges. To our Encephalitis411 community members, we invite you to let us know what emotions the poem evokes for you, or send in a poem of your own to [email protected]. Normal for ageGood news beamed the doc no sign of dementia
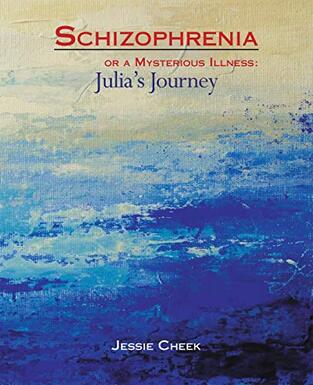
what? hasn’t he read his own referral? assess cognitive defects from encephalitis oh yes pretty well normal for age sudden memory loss normal for age? I don’t want to be normal for age I’m a chess player and he says wonderful you can still play snakes and ladders the beam shifted well that’s all good isn’t it was there anything more? And that was that you break a leg they give you a crutch you break a brain then you’re on your own if you’re normal for age and the nine year old beats you at chess and you pretend you’ve let him win but you do look normal and if another friend patronises you we’re all forgetting things at our age you’ll wring his scrawny neck within and smile happily without and retire early ‘to pursue other interests’ the job too demanding for normal for age and hear them say not pulling his weight not seeing the leaden lumbered uphill pedalling ever paddling beneath But my intellect is not me my processing speed is not me those one time overproud possessions lost to a marauding virus cerebral kenosis revealing the real me is more a seeing afresh friends family strangers that lorikeet now upside down feeding and grandma’s hundred year old lavender still blooming I laugh with you cry with you and if my jigsaw pieces keep falling out and if I get lost in once familiar streets does it really truly matter? a never expected silver lined gift of freedom thank you I say and shake hands with that old virus or go outside and scream at the silent moon or swallow the sweetened lure and wallow in the lost and once was me INTRODUCTION TO THE CHEEK'SFor over a decade, the Cheek’s have been on a long journey with a strange illness that was misdiagnosed as schizophrenia. It took years of doctor’s visits, advocacy, and persistence as a family in order to unravel the mystery of what Julia Cheek (bottom left in the photo above) needed to heal. Julia’s story is an illustrative case of how complex it can be to diagnose, treat, and recover from autoimmune encephalitis (AE). While classic cases of AE present suddenly with a myriad of neuropsychiatric symptoms, there have also been occasional reports of AE that present with a slower onset or with isolated psychiatric symptoms. There may be fewer lab or imaging abnormalities than typical, and no identified autoantibody; but these patients have nonetheless responded dramatically to immunotherapies. Julia’s mother, Jessie Cheek, captures the harsh realities of having an unusual case of seronegative AE in her book Schizophrenia or a Mysterious Illness: Julia’s Journey. Jessie is a rare disease advocate who generously shares her knowledge with others, provides support to those who could use encouragement, and fosters connections between community members. We’re delighted she wrote this blog post for Encephalitis411, which shines a light on just how variable encephalitis can look! An Unusual Case of seronegative autoimmune Encephalitis: Julia's StoryBy jessie cheekAs I write this, Julia Cheek is 27 years old. My husband, Mike and I never expected that our daughter would ever have any health issues. She was a happy, healthy, and bright little girl, but once she hit puberty, her personality began to change slowly. Her symptoms developed very gradually, unlike the experience of many other encephalitis survivors. Early signs of troubleJulia began struggling a little with her schoolwork in 2008, but by the time she was in her sophomore year of high school in 2011, her grades slipped drastically, and she began to exhibit strange mannerisms. We brought her home to home-school her, and discussed her situation with her pediatrician, but Julia continued to decline mentally and emotionally. She withdrew from social interactions and seemed to be reacting to internal thoughts. She told me that her imaginations seemed to be taking over her life. When ADHD treatments, counseling for fantasy addiction and other therapies didn’t work, we began seeking other doctors for help. After consulting neurologists, endocrinologists, pulmonologists, and psychiatrists, we still had no answers. The psychiatrists thought she had an underlying medical problem, and told us that we needed to find a more curious doctor. Meanwhile, Julia continued to decline until she had a complete psychotic break. the Psychotic Break and Misdiagnosis of SchizophreniaIn September 2013, Julia’s first psychotic episode began with a severe stomach ache and headache. She was catatonic by the time she arrived in the ER, but she was not admitted into the hospital. The hospital’s diagnosis was depression and thyroid issues. At 3 a.m. we were told to take her home and find a new neurologist and psychiatrist. Everyone in the family went to sleep, except for Julia. Julia left the house at 4 a.m. and, after crossing a busy street into another neighborhood, began banging on a stranger’s door. The police were called, and at 5:30 a.m. we received a phone call from a police officer. We had been sleeping and did not know she had left the house. She still had on her identification bracelet from the hospital and she remembered her phone number, but when the officer brought her home she declared that she was our adopted daughter and that her real name was Rebecca Jones. She had many other delusions as well. We admitted her into a local psychiatric hospital where she was misdiagnosed as having schizophrenia. Her local psychiatrist gave her medications for schizophrenia but they didn’t help her much. After seeing another neurologist, another endocrinologist and a new primary care doctor, many more tests were run. Her new primary care doctor and her psychiatrist told us to take Julia to the Mayo Clinic in Rochester, Minnesota. Digging Deeper for AnswersIn January 2014, Julia spent many days at the Mayo Clinic, but the staff could not find any organic cause for her symptoms. Her MRI and PET imaging scans of the brain, electroencephalogram (EEG), bloodwork and cerebrospinal fluid were mostly normal. For a few hours after her lumbar puncture she seemed to regain some normalcy. She talked to us that evening, cried and asked us when the doctors were ever going to figure out what was wrong with her body. It seems that the pressure released by the lumbar puncture had helped relieve the pressure in her brain. But by the next morning, she had returned to her non-communicative self and the doctors had not been able to observe the temporary change in her demeanor, so most of the doctors did not think that event was significant. Her Houston psychiatrist though told me to emphasize this event in all of my follow-up visits with other neurologists. The Mayo Clinic doctors did not think she was in the beginning stages of schizophrenia. They provided the diagnoses of psychosis (non-specific), likely delusional disorder, and idiopathic hypersomnolence. The doctors thought she might have a developmental disability as well, but didn’t know what it was. The doctors wouldn’t rule out an organic cause, but they couldn’t pinpoint anything. We came back to Houston, her doctors ordered more tests, but Julia continued to decline. A new endocrinologist decided that Julia had Hashimoto’s. Julia kept declining to where she could no longer change her clothes, shower, or eat or drink without lots of prodding. She was in the ER twice for dehydration. She was very irritable and hardly spoke to anyone in the family. We wondered if Julia would ever be happy and fully functioning again. We had many of our friends praying for her and, at our church, a special prayer meeting was held for her healing. The Steroid TrialOne of the Mayo Clinic doctors suggested that we could have Julia try a round of steroids to see if there would be any improvement. After the doctors had run out of other tests to give her, I asked her neurologist to prescribe some steroids for her. If I had known what I know now, I would have asked for high dose steroid infusions, but he prescribed 40 mg/day oral steroids for a month. Finally, Julia did show some improvement. She began to be able to eat, drink, shower and dress herself again. After one month, the doctor wanted to taper from the steroids, but I begged him to try again for another month. Meanwhile, I was talking to other doctors and corresponding with many other people. I heard about the Undiagnosed Diseases Network that would have a new site in Houston. When Julia continued to experience small improvements on steroids, it was recommended that we contact the Mayo Clinic again. The local neurologist agreed to allow Julia to continue the steroids while we waited for our Mayo Clinic appointment, this time with a specialist in the adult neuro-immunology department. Finding Accurate DiagnosesIn August 2014, Julia was officially diagnosed by the Mayo Clinic doctors with sub-acute autoimmune encephalopathy and Hashimoto’s thyroiditis. She was given Imuran and IVIG infusions. We finally had hope. It took about a year before Julia could begin to manage all of her homeschool subjects again, but she eventually managed to complete all of her high school studies in 2017. In 2016, Julia was admitted into the Undiagnosed Diseases Network where she was given the further diagnosis of Coffin-Lowry syndrome (CLS). CLS is caused by a rare gene mutation and can present as craniofacial abnormalities, progressive skeletal abnormalities, intellectual disability, and behavioural challenges. We were told that Julia was the only known medical case of a patient having CLS as well as autoimmune encephalitis (AE). I wondered if there was a connection between her CLS gene mutation and her AE. Immunosuppressant Treatments and OutcomesSince 2014, Julia has been on continuous bi-weekly IVIG treatments and Imuran. When she had difficulty with weaning from the prednisone, a rare disease specialist suggested adding yet another immunosuppressant to her medications. She began taking CellCept in 2018, which enabled her to become prednisone-free. Unfortunately the many years of prednisone added about 80 pounds to her weight, which she has been unable to lose. Julia has no more delusional thinking and has continued to improve over the years. She has no memory loss except for what happened to her when she was so very sick. Her main residual symptom is chronic fatigue. I have written a book about Julia’s medical journey, called Schizophrenia or a Mysterious Illness: Julia’s Journey. Attending College, Making Friends, and Living Live Beyond EncephalitisJulia was able to complete her Associate in Arts degree in 2020 and is currently working on an online Bachelor’s degree in Creative Writing at Colorado Christian University. She is pursuing her many hobbies and enjoys social interactions again. It took a long time for her brain to heal again and an even longer time for her emotions to heal. Today Julia is happy again, and we are so very thankful. She had lost contact with her best friend from high school, but today they chat regularly and even though she now lives in another state, Jessica recently came for a visit. Julia now uses her imagination in positive ways and recently used it to fix up her room. She is enjoying her Creative Writing classes and clubs, and looks forward to writing her own book one day. Connecting with Others in the Rare Disease CommunityDuring Julia’s healing journey, our family has met other survivors of autoimmune encephalitis and one step in Julia’s healing was when she consented to go with me to visit Sha Conerway. Julia was at first very reluctant to talk to anyone about what she had experienced with encephalitis, but now she wanted to begin helping someone else. Julia’s story encouraged Sha’s family. We helped Sha find a good doctor and we prayed for Sha to be healed also. After Sha recovered from AE we visited with her. Sha has also written a little book about her experience with AE called Grateful. After publishing my book about Julia’s journey, I began to hear from other Coffin-Lowry syndrome (CLS) families and a number of them seemed to have daughters whose stories sounded eerily similar to Julia’s story. Several of them are now looking to pursue doctors in order to be evaluated for AE. I still wonder if the Coffin-Lowry gene mutation might have contributed to Julia’s AE, but there is currently no medical literature that links these two rare diseases.  In the summer of 2022, our family was able to attend a conference where Julia could meet other young people with Coffin-Lowry syndrome. Several of the people at the Coffin-Lowry Syndrome conference were wearing this t-shirt. I think the same could be said about autoimmune encephalitis. I had had a miscarriage a few months before I became pregnant with Julia, so I was concerned that I might have another miscarriage. A verse in the Bible was very meaningful to me during this time. Philippians 1:6. “He who began a good work in you, will be faithful to complete it.” During those years when Julia was so very ill, I kept wondering how God was going to work in Julia’s life. This verse continues to encourage me as I see how much Julia has healed during the past eight years. Her current primary care doctor recently told us that she has continued to notice improvements and ongoing healing even during the past four years since she was stable enough to begin college. We are so thankful. overcoming Autoimmune EncephalitisOver the years, Julia’s doctors have referred to her illness by several different names. Initially she was diagnosed with sub-acute autoimmune encephalopathy. Other doctors call it autoimmune encephalitis. Some call it steroid responsive encephalitis or even Hashimoto’s encephalitis. Today the term seronegative autoimmune encephalitis is often used to describe patients like her. Doctors seem to disagree on exactly the correct label. Some doctors even believe her condition is different because of her Coffin-Lowry syndrome.
Whatever the exact name, Julia seems to have some form of autoimmune encephalitis that has responded very well to immunosuppressant medication. Though it’s been a long and slow journey, we are thankful for her continued healing over many years. Introduction to Linda and colton"My son was diagnosed with E at the age of 1, we were told first that he wouldn’t survive, then we were told he would never walk or talk... Flash forward to today, I just wanted to share that with support, lots of hard work and his determination, he is a freshman in college and a collegiate athlete (lacrosse). He’ll live with his brain injury the rest of his life, but just wanted to share that there is hope, there is support and there are miracles." ~Linda Fereira, a long-time Inspire.com member Encephalitis411's origins go back well over a decade, to when founders Becky Dennis and Bob Morris met while serving on the board of Encephalitis Global (which later became a part of Encephalitis411). Back then, there were fewer resources and ways to meet others in the encephalitis community. Most met through the Inspire.com forum, which has a rich history of conversation and knowledge that can still be accessed today. Linda, a long-time community member who some may recognize from Inspire.com, recently caught up with us to provide an update on her son. For anyone looking for hope and inspiration, this is it! It's not too often that we get updates from those who were active in the community's earliest days, which makes her uplifting testimony all the more memorable. We are so proud of Colton and hope you'll join us in celebrating his successes by reading his story below. a testimony years in the making |
| Things rapidly changed overnight as Colton began to have seizures and fell into a coma. I rushed to the hospital that next morning only to be met by my husband and our pastor. The doctors had told my husband that they didn’t expect Colton to survive and that we should begin planning for his funeral. |
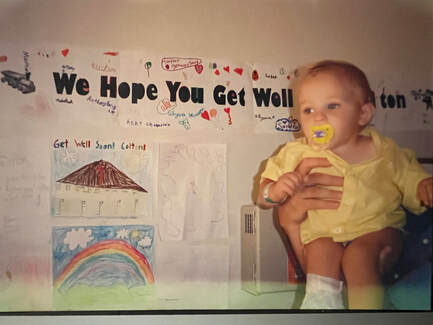
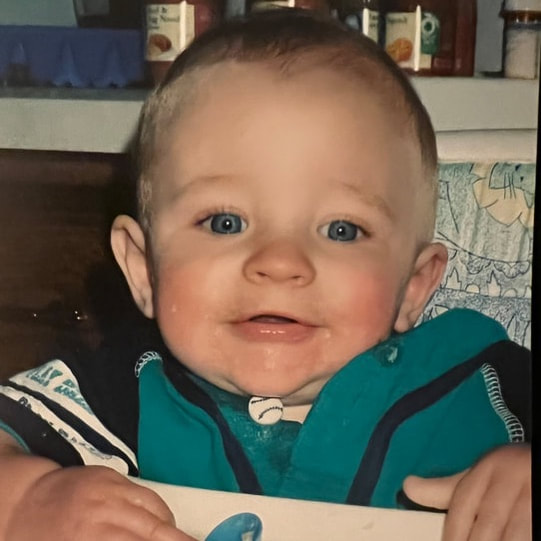
He was moved to the PICU and hooked up to monitors and had so many tests run. Days into this as he held on, it was finally determined that he had encephalitis. Possible cause, his chickenpox vaccine. He remained in a coma for almost a week. We were told that if he survived he would never walk or talk. After 10 days he woke from the coma. He was up, he was walking and playing. He did need to relearn things, such as walking and feeding himself with things like banana pieces and such.
| We were sent home on seizure medication, visits from the Center for Disease Control and Prevention, and in-home occupational and physical therapy. They worked on his motor skills and his speech. He seemed to be recovering at a rapid pace and was soon running and jumping and doing all the things that he had done before falling sick. After six months he was off all medications. Over the next few years, he seemed to be a healthy, happy toddler. |
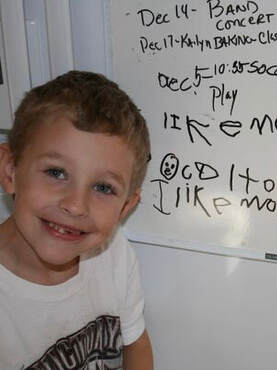
As he turned five and we began to prepare him for school we noticed a few things such as his not being able to tie his shoes or button his clothes, and often he would tell us “I forgot” when things we asked him to do were not done. None of this alarmed us, after all, what child doesn’t tell you they forgot when they get sidetracked while playing, etc?
His kindergarten and first-grade teachers noticed things that caused the concern. They would tell us that Colton would pay attention to things that were being said, but would often stare at his desk not being able to comprehend what he needed to do. He was struggling to learn to read. They suggested we get him tested.
Tests showed that Colton had damage to an area of his brain that caused short-term memory loss. He also had no feeling in his fingertips, which solved the problem of why he couldn’t button his clothes or tie his shoes. He actually tested so low in school that they suggested we place him in Special Education. We refused.
His kindergarten and first-grade teachers noticed things that caused the concern. They would tell us that Colton would pay attention to things that were being said, but would often stare at his desk not being able to comprehend what he needed to do. He was struggling to learn to read. They suggested we get him tested.
Tests showed that Colton had damage to an area of his brain that caused short-term memory loss. He also had no feeling in his fingertips, which solved the problem of why he couldn’t button his clothes or tie his shoes. He actually tested so low in school that they suggested we place him in Special Education. We refused.
We got tutors, used horse therapy, and continued to help him in any way we could to keep him moving forward. Slowly he made progress and we as a family learned to deal with his memory loss issues.
Colton went on to make the honor roll through middle school. He participated in different sports, including baseball, wrestling, soccer, football and finally lacrosse. His playing lacrosse led to him being offered a position on a college team and fulfilling his dream of being a college athlete.
Colton will live with his short-term memory loss for the rest of his life. He will also continue to have to work with the lack of feeling in his fingertips. He has never let either of these stand in his way. Most people who meet him have no idea that there ever was or is a problem. We couldn’t be more grateful for his life. Never will I forget the feeling of despair that I felt that day they told us to prepare for his funeral, nor will I take for granted the life he has gone on to live.
Encephalitis took many things from his childhood, but in his journey to overcome it, Colton has become a story of strength and survival.
‘Tis the season for parties, get-togethers, Christmas concerts, work socials, school performances, and a range of other holiday festivities.
Great, you might be thinking. Here comes another thing to add to the calendar before the year is over.
But this is one invitation you don’t have to spend hours preparing for. In fact, your presence is not even requested.
You can simply let your hair down, throw on your comfy pajamas, sip a warm tea, curl up under a warm blanket, and join the club of us who could use a reason to slow down this holiday season.
As the year draws to a close, we at Encephalitis411 invite you to view Fighting Encephalitis Head On!, a short video that features a few stories from our community.
As you watch, take a moment to step back from the hustle and bustle of the year and reflect on the things that matter most to you.
Great, you might be thinking. Here comes another thing to add to the calendar before the year is over.
But this is one invitation you don’t have to spend hours preparing for. In fact, your presence is not even requested.
You can simply let your hair down, throw on your comfy pajamas, sip a warm tea, curl up under a warm blanket, and join the club of us who could use a reason to slow down this holiday season.
As the year draws to a close, we at Encephalitis411 invite you to view Fighting Encephalitis Head On!, a short video that features a few stories from our community.
As you watch, take a moment to step back from the hustle and bustle of the year and reflect on the things that matter most to you.
Fighting Encephalitis Head On!
For many of us, health, family, and friendships top the list of things we cherish most. Yet these are often the areas that become destabilized most for those who are impacted by encephalitis. Every day we support and advocate for individuals experiencing the devastating physical, economic, and psychosocial consequences of encephalitis.
Next year will be no different. Looking ahead to 2023, 20,000 people in the U.S alone will be diagnosed with encephalitis. That’s a new town of people who will be unexpectedly faced with the harsh realities of fighting to get care for a rare disease that is frequently misdiagnosed, has no cure, is poorly understood by the medical community, and forever changes the lives of those it touches.
And they’re going to need our support.
We know that many are facing financial hardship during these challenging economic times. Further still, some are struggling under the weight of medical debt due to the lack of FDA-approved medications to treat encephalitis, and the numerous barriers to insurance coverage for critical rehabilitative therapies.
That’s why we at Encephalitis411 strive to keep our services 100% free. We are honoured to support patients, caregivers, medical providers, and other community members during their critical times of need.
But for those in more fortunate circumstances, we would appreciate your support. Please consider making a tax deductible donation before the end of the year, to enable us to continue these vital services for those impacted by encephalitis.
Next year will be no different. Looking ahead to 2023, 20,000 people in the U.S alone will be diagnosed with encephalitis. That’s a new town of people who will be unexpectedly faced with the harsh realities of fighting to get care for a rare disease that is frequently misdiagnosed, has no cure, is poorly understood by the medical community, and forever changes the lives of those it touches.
And they’re going to need our support.
We know that many are facing financial hardship during these challenging economic times. Further still, some are struggling under the weight of medical debt due to the lack of FDA-approved medications to treat encephalitis, and the numerous barriers to insurance coverage for critical rehabilitative therapies.
That’s why we at Encephalitis411 strive to keep our services 100% free. We are honoured to support patients, caregivers, medical providers, and other community members during their critical times of need.
But for those in more fortunate circumstances, we would appreciate your support. Please consider making a tax deductible donation before the end of the year, to enable us to continue these vital services for those impacted by encephalitis.
other ways to give
- Behind on your holiday gift shopping? Make a charitable donation in the name of your gift recipient(s). On the donation page you can select “Make this a Tribute Donation” and customize an e-card that will be sent to your gift recipient from Encephalitis411.
- Hard to shop for or already have everything you need? Set up a personal Facebook fundraiser for Encephalitis411. It’s a win-win solution for those who struggle to answer the question, “What do you want for Christmas this year?” For step-by-step instructions on how to set up a Facebook fundraiser, visit this page.
- Want to help raise awareness? Browse our Encephalitis411 merchandise and pick out some items that can be used at school, at the office, or out running errands.
- Ordering from Amazon? Use our Amazon Smile link to support Encephalitis411. A portion of every purchase will be donated to our organization, at no additional cost to you.
We appreciate each and every one of you who has been a part of our community this year. Thank you for your support and happy holidays from all of us at Encephalitis411!
"I’ve relearned to walk, talk, and see, with lots in between. I’d love to get my story out there.” ~Elissa Campbell, 2019 viral encephalitis and viral meningitis survivor
Encephalitis411 first met Elissa when she signed up to Wipe Out Encephalitis during this year’s Nicole’s Challenge: The Walk to Cure Encephalitis. We’re proud to have her as part of the Encephalitis411 community; and to help her celebrate how far she’s come, we’re sharing her story on the 3 year anniversary since her medical journey began.
Please find Elissa’s words below and join us in celebrating her strength, courage, and positive spirit.
Please find Elissa’s words below and join us in celebrating her strength, courage, and positive spirit.
2019: The beginning

On November 14, 2019, I was seen in the Northside Hospital emergency room in Cumming, Georgia for dizziness. Due to my work travel for the last 5 weeks, it was determined to be vertigo and I was released. I did vertigo relief exercises and acupuncture twice to try to help.
On 11/17/2019, my husband drove me back to the acupuncturist as my symptoms had worsened. As we left, he had to carry me as I could no longer walk and my speech was severely slurred. Thankfully, he took me to the hospital again and this time I was admitted.
This is where my journey to finding answers and healing began.
By 11/19/2019, I had 3 MRI scans, 2 of them with contrast. I was started on antibiotics to throw anything at whatever this was to help. My rounding neurologist could not find anything with the results of the MRIs and bloodwork. My symptoms worsened as now I could not walk, talk, see, or keep food down.
On 11/20/2019, my rounding Infectious Disease (ID) physician insisted on a lumbar puncture (LP) in a further attempt to find answers. She started me on intravenous immune globulin (IVIG) also. This was a 5 day infusion that was administered along with antibiotics. My husband, daughters, and sisters sat around the clock with me to assist in helping me get up for basic needs. I had to be assisted in walking, eating, using the restroom and eventually showering. I was poked and prodded for daily bloodwork and more MRIs (9 in total) to try to see anything.
By 11/27/2019, results from the LP and MRI finally resulted in the diagnosis of viral encephalitis that settled in the mid brain and brain stem, viral meningitis, and to top it off, IgG (old) antibodies of Lyme disease. It was a go big or go home scenario. The viruses debilitated me and the Lyme slowed my ability to recover.
11/28/2019 was Thanksgiving. A ton to be thankful for including finally being diagnosed, friends and family, medical staff, and my faith to carry me. My family enjoyed Thanksgiving dinner from my hospital room and I attempted (to no avail) to eat and keep it down.
On 11/29/2019, I had a double lumen PICC line (central venous catheter) put in my chest and orders to be moved to a local rehab facility (overnight stay) so I could receive constant occupational therapy (OT), physiotherapy (PT), and speech language pathology (SLP) therapy.
On 11/20/2019, my rounding Infectious Disease (ID) physician insisted on a lumbar puncture (LP) in a further attempt to find answers. She started me on intravenous immune globulin (IVIG) also. This was a 5 day infusion that was administered along with antibiotics. My husband, daughters, and sisters sat around the clock with me to assist in helping me get up for basic needs. I had to be assisted in walking, eating, using the restroom and eventually showering. I was poked and prodded for daily bloodwork and more MRIs (9 in total) to try to see anything.
By 11/27/2019, results from the LP and MRI finally resulted in the diagnosis of viral encephalitis that settled in the mid brain and brain stem, viral meningitis, and to top it off, IgG (old) antibodies of Lyme disease. It was a go big or go home scenario. The viruses debilitated me and the Lyme slowed my ability to recover.
11/28/2019 was Thanksgiving. A ton to be thankful for including finally being diagnosed, friends and family, medical staff, and my faith to carry me. My family enjoyed Thanksgiving dinner from my hospital room and I attempted (to no avail) to eat and keep it down.
On 11/29/2019, I had a double lumen PICC line (central venous catheter) put in my chest and orders to be moved to a local rehab facility (overnight stay) so I could receive constant occupational therapy (OT), physiotherapy (PT), and speech language pathology (SLP) therapy.
11/30/2019 was my first full day of rehab and they were able to get me to use a walker for 17 ft, even further with the wheelchair. This was a 3 week journey of relearning to do simple tasks of brushing teeth, using the restroom, showering, etc. Keeping food down was still a challenge. I continued daily infusions of antibiotics (Rocefin) and Heparin shots in the abdomen since I was still spending most of my time in bed.
12/20/2019 was the best early Christmas present—I got to come home! Mainly using the wheelchair but still learning the walker, and my husband caring for my needs with showering, etc.
12/20/2019 was the best early Christmas present—I got to come home! Mainly using the wheelchair but still learning the walker, and my husband caring for my needs with showering, etc.
2020: Recovery at home
At home, I continued to have PT come to the house to work with me and my recovery. I was mainly under the care of my ID and having daily infusions of the antibiotic—for 13 weeks daily. I also had weekly visits at my ID office. At the same time, I began working with a Lyme Literate Doctor (LLMD) to combat the Lyme disease. He felt a treatment of Supportive Oligonucleotide Therapy (SOT) was worthwhile to pursue. It’s pretty fascinating to learn about. I have the sweetest family and friends who set up a GoFundMe page because it is a very costly therapy.
I also started boosting my gut health and immune system with Myer’s Cocktail infusions and other natural infusions of vitamins. Typically 2x weekly for about 6 months.
2/27/2020 I finished my 13 weeks of antibiotic infusions and had PICC line removed.
3/13/2020 I received my SOT infusion! This should and hopefully did stop the replication of cells infected with Lyme.
March was also the month I started showering myself. YAY!
By 5/2020, my speech had improved to nearly 100%, and I had stopped using my wheelchair and walker and graduated to a cane. I was very unsteady but determined to become independent. I also started attempting to drive to close by spots, including doc appts within 5 mins away. I was still doing PT and aquatic therapy.
On 9/25/2020 I graduated from PT. Not because I was great but because I had all of the tools to continue improving on my own.
I also returned to work full-time.
I also started boosting my gut health and immune system with Myer’s Cocktail infusions and other natural infusions of vitamins. Typically 2x weekly for about 6 months.
2/27/2020 I finished my 13 weeks of antibiotic infusions and had PICC line removed.
3/13/2020 I received my SOT infusion! This should and hopefully did stop the replication of cells infected with Lyme.
March was also the month I started showering myself. YAY!
By 5/2020, my speech had improved to nearly 100%, and I had stopped using my wheelchair and walker and graduated to a cane. I was very unsteady but determined to become independent. I also started attempting to drive to close by spots, including doc appts within 5 mins away. I was still doing PT and aquatic therapy.
On 9/25/2020 I graduated from PT. Not because I was great but because I had all of the tools to continue improving on my own.
I also returned to work full-time.
Facebook post - November 17, 2020:
One year ago I started a journey I never expected! Most know but some do not. What started out as thinking it was vertigo ended up with viral meningitis, encephalitis in the brain stem, and Lyme disease - mimicking a stroke. This left me unable to walk, talk, or see. I’m so thankful to be here a year later to tell my story and help anyone that may be in similar circumstances. So many blessings and so much love to spread! Thank you Colin J. Campbell, Catie Campbell, Evie Campbell, Lynn Walker Kirby, Steve Kirby, Stacey Walker Stanley, Michelle Simmons Payne, and Catriona Campbell for loving/caring for me like I never imagined! Thank you quarantine for allowing everyone to be with me during my recovery! My care took so many people - family, friends, healthcare heroes - and so much love. A year of infusions, many MRIs, PT, OT, and SLP dropped so many angels in my path! And I met the sweetest people to help with doors, elevators, and everything in between while trying to get the hang of a wheelchair, a walker, and unsteady walking. I was also able to participate in specialized treatment with everyone’s support. Since this, I have improved and I can almost walk without struggle. Through this all, God has carried me, guided me, made sure I’m cared for, and lit my road to recovery!
I’m not sure what the future holds nor do I know God’s use for this journey, but I’m certain I will know soon and proudly do as I’m led.
1 Peter 5:10 And the God of all grace, who called you to his eternal glory in Christ, after you have suffered a little while, will himself restore you and make you strong, firm and steadfast.
One year ago I started a journey I never expected! Most know but some do not. What started out as thinking it was vertigo ended up with viral meningitis, encephalitis in the brain stem, and Lyme disease - mimicking a stroke. This left me unable to walk, talk, or see. I’m so thankful to be here a year later to tell my story and help anyone that may be in similar circumstances. So many blessings and so much love to spread! Thank you Colin J. Campbell, Catie Campbell, Evie Campbell, Lynn Walker Kirby, Steve Kirby, Stacey Walker Stanley, Michelle Simmons Payne, and Catriona Campbell for loving/caring for me like I never imagined! Thank you quarantine for allowing everyone to be with me during my recovery! My care took so many people - family, friends, healthcare heroes - and so much love. A year of infusions, many MRIs, PT, OT, and SLP dropped so many angels in my path! And I met the sweetest people to help with doors, elevators, and everything in between while trying to get the hang of a wheelchair, a walker, and unsteady walking. I was also able to participate in specialized treatment with everyone’s support. Since this, I have improved and I can almost walk without struggle. Through this all, God has carried me, guided me, made sure I’m cared for, and lit my road to recovery!
I’m not sure what the future holds nor do I know God’s use for this journey, but I’m certain I will know soon and proudly do as I’m led.
1 Peter 5:10 And the God of all grace, who called you to his eternal glory in Christ, after you have suffered a little while, will himself restore you and make you strong, firm and steadfast.
2021
2021 was a year that I continued to improve on stability and relearn functions not used daily. I realized I couldn’t sing or whistle. These and many more tasks just took focus and determination to relearn. It still remains very tiring. I have to tell my brain to tell my feet to step up for a curb or step over a puddle. Things just weren’t automatic for me.
2022
Fast forward to 1/10/2022, COVID positive and started losing motor skills. Neurologist stated this will always happen with any virus. WHAT???
I had the monoclonal antibody infusion and started back with PT. What I realized is PT continued to work on strength. That is one item I never lost. I lost the ability to do tasks. My brain could not tell my body what to do.
SO… I stopped PT and joined a gym: Orange Theory. This has been phenomenal!! If I can’t figure out an exercise, they give me modifications until I can figure them out.
I also have returned to my kinesiologist for help and sought inflammation reflexology technology (IRT) to take care of any inflammation remaining in my brain. I feel I am closer to being myself, recognizing I have a new normal.
This week marks my 3 years on this journey. (And my 100th Orange Theory class :)) I am so blessed to be here!
I had the monoclonal antibody infusion and started back with PT. What I realized is PT continued to work on strength. That is one item I never lost. I lost the ability to do tasks. My brain could not tell my body what to do.
SO… I stopped PT and joined a gym: Orange Theory. This has been phenomenal!! If I can’t figure out an exercise, they give me modifications until I can figure them out.
I also have returned to my kinesiologist for help and sought inflammation reflexology technology (IRT) to take care of any inflammation remaining in my brain. I feel I am closer to being myself, recognizing I have a new normal.
This week marks my 3 years on this journey. (And my 100th Orange Theory class :)) I am so blessed to be here!
What I've learned
What I have found out, I (and my family) am/are my own advocate(s). No one really knows what is going on in my brain as this is not a typical journey.
I wish I knew a “me” when this all started so I could know stuff to help. I do have a new brain with a TBI now.
I have taken all paths with medicine and have a healthy blend of western and eastern medicine. Sleep is my friend and if I need to stop a second, I do.
My mental health is so important and I listen to my head, my heart and my body.
My faith in God has given me the strength to move on. He has provided in all ways for my healing.
My family and friends are my cheerleaders and mean the world to me. I cannot thank them enough!
I wish I knew a “me” when this all started so I could know stuff to help. I do have a new brain with a TBI now.
I have taken all paths with medicine and have a healthy blend of western and eastern medicine. Sleep is my friend and if I need to stop a second, I do.
My mental health is so important and I listen to my head, my heart and my body.
My faith in God has given me the strength to move on. He has provided in all ways for my healing.
My family and friends are my cheerleaders and mean the world to me. I cannot thank them enough!
Proper care for rural patients in America poses a real challenge. Imagine suffering a brain injury and the nearest city of 100,000 residents or more is 3 hours away. I use this specific population because in the U.S., it almost always requires this size of city to fully represent the sufficient amount of healthcare disciplines required for complex illnesses, such as encephalitis, inflammation of the brain.
While we’re on the topic of hurricanes in the “cone of uncertainty,” let’s talk about how encephalitis (swelling of the brain) mimics this uncertainty.
Written February 21, 2016
Encephalitis. What a mouthful of a word. Ever heard of it? I hadn’t heard of this 12-letter word until 6 years ago. When the doctor said it, I kinda shrugged, thinking “thank God it wasn’t a stroke.” His expression changed as he explained that encephalitis is a form of brain injury, quite similar to a stroke.
“Huh?!” He broke down the word for me … encepha = brain and itis = swelling, therefore encepha + itis = swelling/inflammation of the brain.
It also = life-time change. When the brain is inflamed, all sorts of damage occurs, impairing memory, vision, balance, sleep, cognition, taste/smell, ability to concentrate and well, I could list another 200 residuals that encephalitis survivors report, including personality change.
Encephalitis. What a mouthful of a word. Ever heard of it? I hadn’t heard of this 12-letter word until 6 years ago. When the doctor said it, I kinda shrugged, thinking “thank God it wasn’t a stroke.” His expression changed as he explained that encephalitis is a form of brain injury, quite similar to a stroke.
“Huh?!” He broke down the word for me … encepha = brain and itis = swelling, therefore encepha + itis = swelling/inflammation of the brain.
It also = life-time change. When the brain is inflamed, all sorts of damage occurs, impairing memory, vision, balance, sleep, cognition, taste/smell, ability to concentrate and well, I could list another 200 residuals that encephalitis survivors report, including personality change.
Since hearing about Robin Williams’ death, I’ve been stunned at my reaction. How can I grieve over someone I never knew? I’ve paused to notice the richness he represents in influencing me and how his tragic death shakes me.


































 RSS Feed
RSS Feed