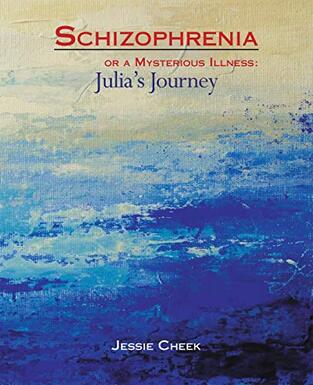
INTRODUCTION TO THE CHEEK'SFor over a decade, the Cheek’s have been on a long journey with a strange illness that was misdiagnosed as schizophrenia. It took years of doctor’s visits, advocacy, and persistence as a family in order to unravel the mystery of what Julia Cheek (bottom left in the photo above) needed to heal. Julia’s story is an illustrative case of how complex it can be to diagnose, treat, and recover from autoimmune encephalitis (AE). While classic cases of AE present suddenly with a myriad of neuropsychiatric symptoms, there have also been occasional reports of AE that present with a slower onset or with isolated psychiatric symptoms. There may be fewer lab or imaging abnormalities than typical, and no identified autoantibody; but these patients have nonetheless responded dramatically to immunotherapies. Julia’s mother, Jessie Cheek, captures the harsh realities of having an unusual case of seronegative AE in her book Schizophrenia or a Mysterious Illness: Julia’s Journey. Jessie is a rare disease advocate who generously shares her knowledge with others, provides support to those who could use encouragement, and fosters connections between community members. We’re delighted she wrote this blog post for Encephalitis411, which shines a light on just how variable encephalitis can look! An Unusual Case of seronegative autoimmune Encephalitis: Julia's StoryBy jessie cheekAs I write this, Julia Cheek is 27 years old. My husband, Mike and I never expected that our daughter would ever have any health issues. She was a happy, healthy, and bright little girl, but once she hit puberty, her personality began to change slowly. Her symptoms developed very gradually, unlike the experience of many other encephalitis survivors. Early signs of troubleJulia began struggling a little with her schoolwork in 2008, but by the time she was in her sophomore year of high school in 2011, her grades slipped drastically, and she began to exhibit strange mannerisms. We brought her home to home-school her, and discussed her situation with her pediatrician, but Julia continued to decline mentally and emotionally. She withdrew from social interactions and seemed to be reacting to internal thoughts. She told me that her imaginations seemed to be taking over her life. When ADHD treatments, counseling for fantasy addiction and other therapies didn’t work, we began seeking other doctors for help. After consulting neurologists, endocrinologists, pulmonologists, and psychiatrists, we still had no answers. The psychiatrists thought she had an underlying medical problem, and told us that we needed to find a more curious doctor. Meanwhile, Julia continued to decline until she had a complete psychotic break. the Psychotic Break and Misdiagnosis of SchizophreniaIn September 2013, Julia’s first psychotic episode began with a severe stomach ache and headache. She was catatonic by the time she arrived in the ER, but she was not admitted into the hospital. The hospital’s diagnosis was depression and thyroid issues. At 3 a.m. we were told to take her home and find a new neurologist and psychiatrist. Everyone in the family went to sleep, except for Julia. Julia left the house at 4 a.m. and, after crossing a busy street into another neighborhood, began banging on a stranger’s door. The police were called, and at 5:30 a.m. we received a phone call from a police officer. We had been sleeping and did not know she had left the house. She still had on her identification bracelet from the hospital and she remembered her phone number, but when the officer brought her home she declared that she was our adopted daughter and that her real name was Rebecca Jones. She had many other delusions as well. We admitted her into a local psychiatric hospital where she was misdiagnosed as having schizophrenia. Her local psychiatrist gave her medications for schizophrenia but they didn’t help her much. After seeing another neurologist, another endocrinologist and a new primary care doctor, many more tests were run. Her new primary care doctor and her psychiatrist told us to take Julia to the Mayo Clinic in Rochester, Minnesota. Digging Deeper for AnswersIn January 2014, Julia spent many days at the Mayo Clinic, but the staff could not find any organic cause for her symptoms. Her MRI and PET imaging scans of the brain, electroencephalogram (EEG), bloodwork and cerebrospinal fluid were mostly normal. For a few hours after her lumbar puncture she seemed to regain some normalcy. She talked to us that evening, cried and asked us when the doctors were ever going to figure out what was wrong with her body. It seems that the pressure released by the lumbar puncture had helped relieve the pressure in her brain. But by the next morning, she had returned to her non-communicative self and the doctors had not been able to observe the temporary change in her demeanor, so most of the doctors did not think that event was significant. Her Houston psychiatrist though told me to emphasize this event in all of my follow-up visits with other neurologists. The Mayo Clinic doctors did not think she was in the beginning stages of schizophrenia. They provided the diagnoses of psychosis (non-specific), likely delusional disorder, and idiopathic hypersomnolence. The doctors thought she might have a developmental disability as well, but didn’t know what it was. The doctors wouldn’t rule out an organic cause, but they couldn’t pinpoint anything. We came back to Houston, her doctors ordered more tests, but Julia continued to decline. A new endocrinologist decided that Julia had Hashimoto’s. Julia kept declining to where she could no longer change her clothes, shower, or eat or drink without lots of prodding. She was in the ER twice for dehydration. She was very irritable and hardly spoke to anyone in the family. We wondered if Julia would ever be happy and fully functioning again. We had many of our friends praying for her and, at our church, a special prayer meeting was held for her healing. The Steroid TrialOne of the Mayo Clinic doctors suggested that we could have Julia try a round of steroids to see if there would be any improvement. After the doctors had run out of other tests to give her, I asked her neurologist to prescribe some steroids for her. If I had known what I know now, I would have asked for high dose steroid infusions, but he prescribed 40 mg/day oral steroids for a month. Finally, Julia did show some improvement. She began to be able to eat, drink, shower and dress herself again. After one month, the doctor wanted to taper from the steroids, but I begged him to try again for another month. Meanwhile, I was talking to other doctors and corresponding with many other people. I heard about the Undiagnosed Diseases Network that would have a new site in Houston. When Julia continued to experience small improvements on steroids, it was recommended that we contact the Mayo Clinic again. The local neurologist agreed to allow Julia to continue the steroids while we waited for our Mayo Clinic appointment, this time with a specialist in the adult neuro-immunology department. Finding Accurate DiagnosesIn August 2014, Julia was officially diagnosed by the Mayo Clinic doctors with sub-acute autoimmune encephalopathy and Hashimoto’s thyroiditis. She was given Imuran and IVIG infusions. We finally had hope. It took about a year before Julia could begin to manage all of her homeschool subjects again, but she eventually managed to complete all of her high school studies in 2017. In 2016, Julia was admitted into the Undiagnosed Diseases Network where she was given the further diagnosis of Coffin-Lowry syndrome (CLS). CLS is caused by a rare gene mutation and can present as craniofacial abnormalities, progressive skeletal abnormalities, intellectual disability, and behavioural challenges. We were told that Julia was the only known medical case of a patient having CLS as well as autoimmune encephalitis (AE). I wondered if there was a connection between her CLS gene mutation and her AE. Immunosuppressant Treatments and OutcomesSince 2014, Julia has been on continuous bi-weekly IVIG treatments and Imuran. When she had difficulty with weaning from the prednisone, a rare disease specialist suggested adding yet another immunosuppressant to her medications. She began taking CellCept in 2018, which enabled her to become prednisone-free. Unfortunately the many years of prednisone added about 80 pounds to her weight, which she has been unable to lose. Julia has no more delusional thinking and has continued to improve over the years. She has no memory loss except for what happened to her when she was so very sick. Her main residual symptom is chronic fatigue. I have written a book about Julia’s medical journey, called Schizophrenia or a Mysterious Illness: Julia’s Journey. Attending College, Making Friends, and Living Live Beyond EncephalitisJulia was able to complete her Associate in Arts degree in 2020 and is currently working on an online Bachelor’s degree in Creative Writing at Colorado Christian University. She is pursuing her many hobbies and enjoys social interactions again. It took a long time for her brain to heal again and an even longer time for her emotions to heal. Today Julia is happy again, and we are so very thankful. She had lost contact with her best friend from high school, but today they chat regularly and even though she now lives in another state, Jessica recently came for a visit. Julia now uses her imagination in positive ways and recently used it to fix up her room. She is enjoying her Creative Writing classes and clubs, and looks forward to writing her own book one day. Connecting with Others in the Rare Disease CommunityDuring Julia’s healing journey, our family has met other survivors of autoimmune encephalitis and one step in Julia’s healing was when she consented to go with me to visit Sha Conerway. Julia was at first very reluctant to talk to anyone about what she had experienced with encephalitis, but now she wanted to begin helping someone else. Julia’s story encouraged Sha’s family. We helped Sha find a good doctor and we prayed for Sha to be healed also. After Sha recovered from AE we visited with her. Sha has also written a little book about her experience with AE called Grateful. After publishing my book about Julia’s journey, I began to hear from other Coffin-Lowry syndrome (CLS) families and a number of them seemed to have daughters whose stories sounded eerily similar to Julia’s story. Several of them are now looking to pursue doctors in order to be evaluated for AE. I still wonder if the Coffin-Lowry gene mutation might have contributed to Julia’s AE, but there is currently no medical literature that links these two rare diseases.  In the summer of 2022, our family was able to attend a conference where Julia could meet other young people with Coffin-Lowry syndrome. Several of the people at the Coffin-Lowry Syndrome conference were wearing this t-shirt. I think the same could be said about autoimmune encephalitis. I had had a miscarriage a few months before I became pregnant with Julia, so I was concerned that I might have another miscarriage. A verse in the Bible was very meaningful to me during this time. Philippians 1:6. “He who began a good work in you, will be faithful to complete it.” During those years when Julia was so very ill, I kept wondering how God was going to work in Julia’s life. This verse continues to encourage me as I see how much Julia has healed during the past eight years. Her current primary care doctor recently told us that she has continued to notice improvements and ongoing healing even during the past four years since she was stable enough to begin college. We are so thankful. overcoming Autoimmune EncephalitisOver the years, Julia’s doctors have referred to her illness by several different names. Initially she was diagnosed with sub-acute autoimmune encephalopathy. Other doctors call it autoimmune encephalitis. Some call it steroid responsive encephalitis or even Hashimoto’s encephalitis. Today the term seronegative autoimmune encephalitis is often used to describe patients like her. Doctors seem to disagree on exactly the correct label. Some doctors even believe her condition is different because of her Coffin-Lowry syndrome.
Whatever the exact name, Julia seems to have some form of autoimmune encephalitis that has responded very well to immunosuppressant medication. Though it’s been a long and slow journey, we are thankful for her continued healing over many years.
1 Comment
Jessie Cheek
3/30/2023 07:11:36 am
My book is now in circulation in the Fort Bend County, TX public library system. Search by author name, Jessie Cheek, for ease of searching in library catalog
Reply
Leave a Reply. |
Content on this site is intended for educational and informational purposes only, and should not be considered medical advice. Always check with your physician for guidance specific to your case.
© Encephalitis411• All rights reserved.
Toll-Free Support Hotline: 1-833-411-3350








 RSS Feed
RSS Feed